The polypill is effective for secondary prevention of cardiovascular disease. By combining drugs in a single pill, it improves convenience and compliance.
The polypill, not polypharmacy. Polypharmacy is the use of multiple medications by a single patient, which is sometimes appropriate and necessary, but can be ill-advised and result in medication interactions and complications. The polypill was first recommended 20 years ago. When the striking ability of statins to reduce the risk of cardiovascular disease was first recognized, one tongue-in-cheek proposal was to add statins to the drinking water. Of course, that scattershot approach didn’t make sense; the dose could not be controlled and would have resulted in over-medicating low-risk patients who didn’t need treatment while under-medicating those who did. And some people don’t drink tap water.
In their original proposal, Wald and Law coined the term polypill to describe a fixed-dose combination of medications to prevent cardiovascular disease. Their proposal was two-fold. They said that giving a polypill to everyone over the age of 55 would reduce cardiovascular events by more than 80%. And they proposed using a fixed-dose combination instead of individually prescribed medications.
A heated debate ensued over who should be treated, and unfortunately it over-shadowed the idea of using a fixed-dose combination, a strategy that has been shown to improve compliance by simplifying the treatment regimen. Re-focusing the debate on secondary prevention removed the objections about giving medication to those who don’t need it, since it has been shown that giving medication to everyone with established cardiovascular disease improves outcomes.
Numerous studies have now shown similar or even improved risk factor control with the polypill as compared to usual care. But previous trials were underpowered and unable to demonstrate the effect of polypills on cardiovascular outcomes. Hence a new study, the SECURE trial, reported in the September 15, 2022 issue of The New England Journal of Medicine, along with an informative editorial by Thomas Wang.
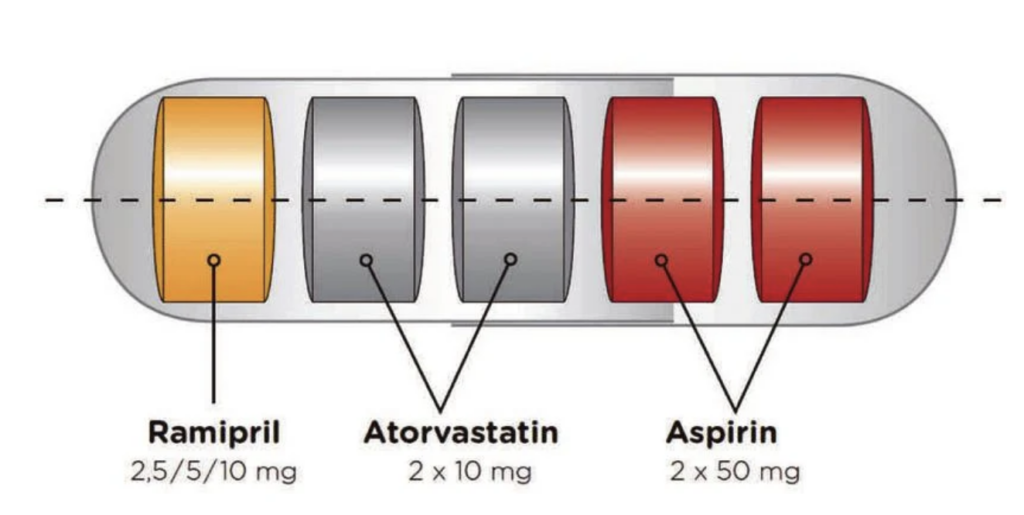
SECURE stands for Secondary Prevention of Cardiovascular Disease in the Elderly. It was an open-label, multinational, randomized, controlled trial comparing a polypill-based strategy (aspirin, atorvastatin, and ramipril) to usual care according to current European Society of Cardiology guidelines for secondary prevention in patients with recent myocardial infarction. 2,500 elderly patients were followed for 3 years. Major cardiovascular events occurred more frequently in the usual care group than in the polypill group (12.7% compared to 9.5%). This was despite high rates of evidence-based therapies in the usual care group (97% were on statins). The safety of the polypill strategy was again confirmed.
Six different formulations of the polypill were available for physicians in the trial to choose from, with 2 different doses of atorvastatin and 3 different doses of ramipril. 95% of patients were also taking a second antiplatelet drug. Should that be added to the polypill to reduce the pill burden even further?
Conclusion: A good idea whose time has come
After 20 years, the polypill’s role in secondary prevention is clear. It improves compliance and outcomes. Some barriers remain, including a lack of commercial interest, but it seems to me a clever marketing campaign could create a blockbuster new drug for some lucky company.
This article was originally published in the Science-Based Medicine Blog.
