There appeared to be an epidemic of melanoma skin cancer, but it seems to be a pseudoepidemic caused by overdiagnosis. Screening everyone with skin exams does more harm than good and can no longer be recommended.
This lesion was suspicious enough to warrant a biopsy, but screening everyone for skin cancer is not warranted. Screening does more harm than good.
In the January 2021 issue of The New England Journal of Medicine, H. Gilbert Welch, Benjamin Mazer, and Adewole Adamson published a “Sounding Board” article entitled “The Rapid Rise in Cutaneous Melanoma Diagnoses“. There appeared to be an epidemic of melanoma, but their careful examination of the evidence revealed it to be a false alarm, a pseudoepidemic. Based on their findings, they recommend that the practice of doing skin examinations to screen for skin cancer be stopped, except for those at substantially high risk.
Melanoma was once rare, but its incidence has increased rapidly and is now 6 times as high as it was 40 years ago. Curiously, this increase is limited to cutaneous melanoma. There has been no increase in noncutaneous melanoma, which has a common cell of origin.
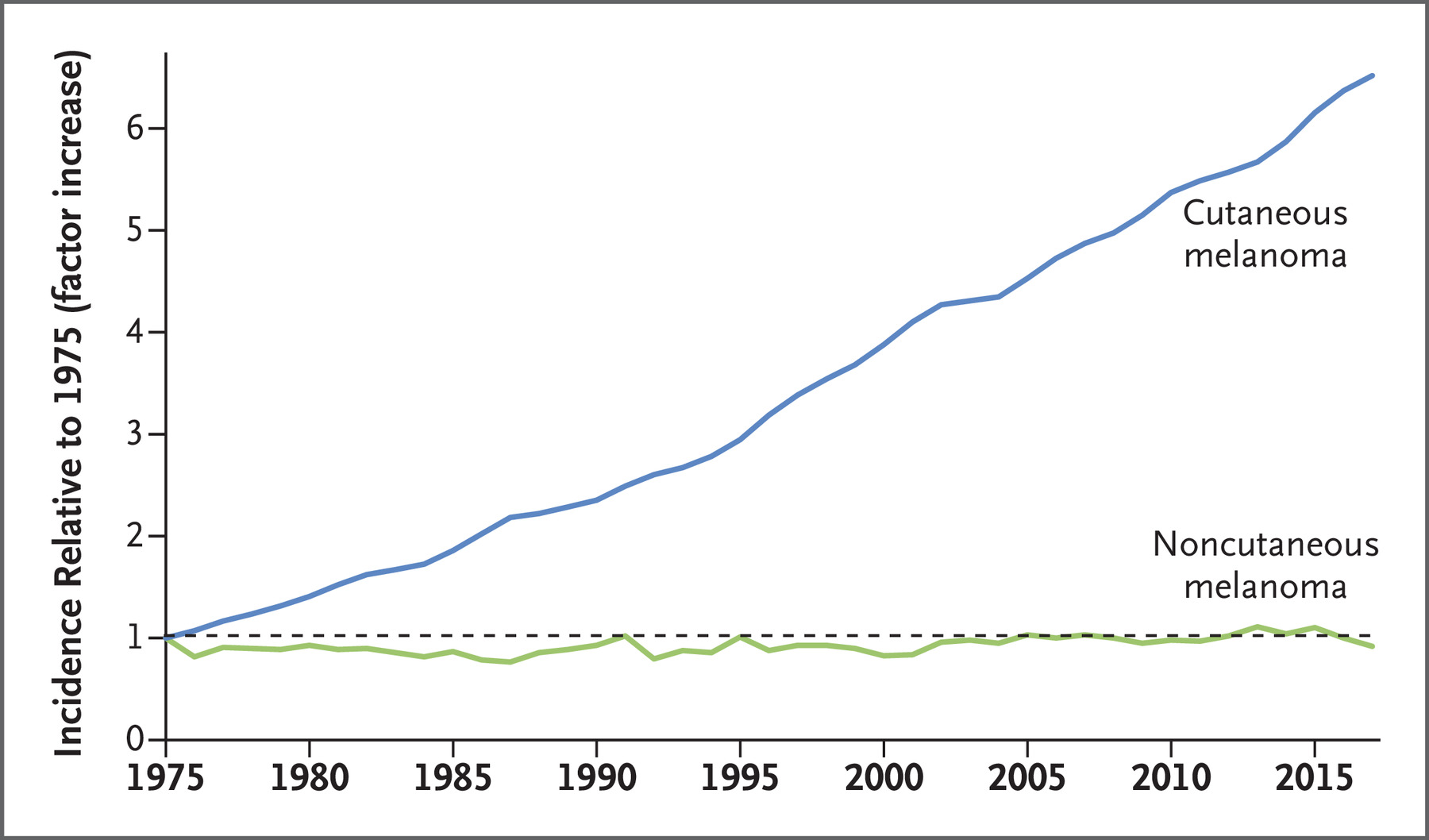
Welch et al. set out to explain this puzzling discrepancy. They had two starting hypotheses: that skin lesions were more accessible to diagnosis, or that the skin was subject to some exposure to which noncutaneous sites were not.
The obvious candidate exposure is ultraviolet exposure from the sun or tanning beds; but the evidence for a relationship between UV radiation and melanoma is mixed, and most of the data come from case-control studies which are subject to recall bias: patients with cancer tend to report more exposure than controls. Total sun exposure carries a 1.34 relative risk of melanoma; chronic sun exposure, a 0.95 relative risk; intermittent exposure, 1.61; sunburn, 2.03; ever having used a tanning bed, 1.2; frequent use of a tanning bed, 1.42; and first use of a tanning bed before the age of 35, 1.59. In short, not a particularly strong association. In the worst possible case, if everyone in the population had been sunburned, we would expect to see a much lower incidence than the 6X increase that was observed.
They found evidence that the increased incidence was due to increased diagnostic scrutiny rather than to UV exposure. During the same time period, almost twice as many Medicare beneficiaries were getting biopsies. The diagnostic criteria are subjective. They found evidence that pathologists have tended to lower thresholds for diagnosing melanoma, and smaller lesions are being biopsied.
Their most compelling argument is that the rise in melanoma diagnoses was not accompanied by a rise in melanoma deaths.
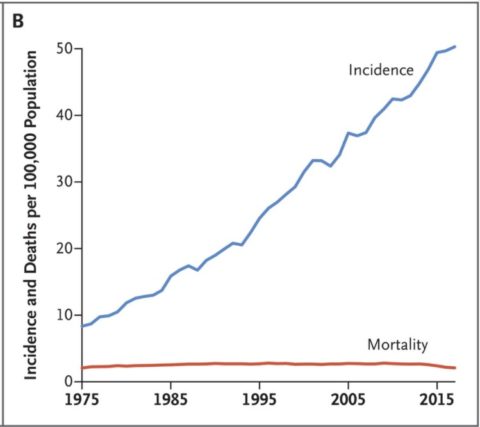
Conclusion: There is no epidemic, but there is a problem of over-diagnosis
They point out “the economic disruption caused by Covid-19 obliges clinicians to protect people from the financial stress of needlessly being turned into a patient”. It gives us an opportunity to change course, to focus on education rather than on screening. Screening everyone for skin cancer does more harm than good and should be stopped.
This article was originally published in the Science-Based Medicine Blog
