TB can’t be diagnosed with a blood test.
Tuberculosis has been infecting humans since prehistoric times. It’s still with us. It usually can be cured today with good medical care but is still a serious problem in much of the world, especially among underprivileged socioeconomic groups and some ethnic populations. It kills 1.5 million people every year, and it’s getting more prevalent because of multi-drug-resistant strains and the interaction with HIV infections. Around 80% of people test positive by skin test in third-world countries, compared to 5-10% of people in the US. If you’re old enough, you may remember getting a tine test in school. A device with multiple short needles coated with TB antigens was pressed into the arm. It had to be read 48-72 hours later by measuring the size of the largest area of induration. It was recommended for testing children because it was easy to use, but it was difficult to control the amount of antigen injected. The Mantoux test, with a single injection, is preferred today, but it also requires a return visit to have it read. Skin tests are also known as PPD tests, for purified protein derivative.
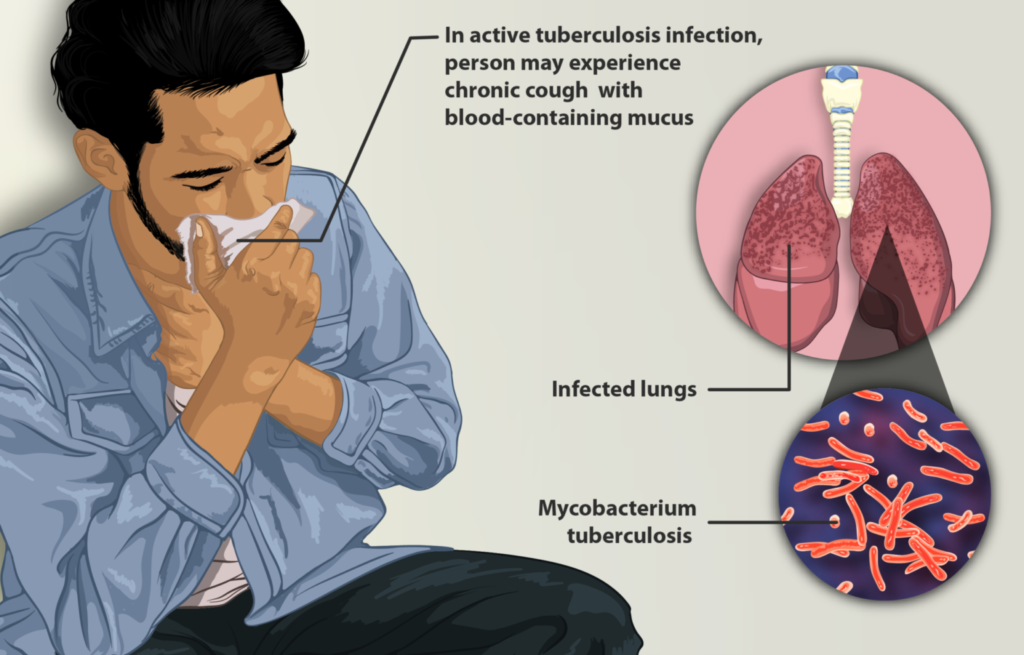
TB has three clinical forms: latent (meaning that they have small numbers of TB bacteria in the body that are alive but inactive and haven’t made them sick or caused any symptoms), pulmonary, and extra-pulmonary and remains a disease difficult to diagnose accurately.
Today there are blood tests for TB. Wouldn’t it be great if a simple blood test could reliably diagnose active TB, with no need for a return visit? Unfortunately, it doesn’t work that way. Many techniques have been tried to diagnose TB, since cultures, the gold standard, are slow and can be unreliable. One test that has gone by the wayside is serology, looking for an antibody response to TB.
In July 2011 the World Health Organization (WHO) issued a warning calling for an end to the practice of doing serologic blood tests for active TB, calling it bad practice because the currently available serologic blood tests are “inconsistent, imprecise and put patients’ lives in danger”. False positive results can occur because other organisms share the same antigens and the antibodies they produce can be confused with antibodies to TB. The blood tests can have false-negative results that falsely reassure patients that they are disease-free, meaning that infected patients will not be treated. After a rigorous review of the data, the WHO found “overwhelming evidence that the blood tests produced an unacceptable level of false results”.
However, new technologies have advanced the diagnosis of latent TB and are of some utility in the complex diagnose of active TB. The two blood tests available in the US that have been approved by the FDA are:
- QuantiFERON®-TB Gold In-Tube test (QFT-GIT)
- T-SPOT®.TB test (T-Spot)
These are Interferon Gamma Release Assay, or IGRAs. The patients lymphocytes are incubated with TB antigens and controls. If the patient has latent or active TB, the lymphocytes will release interferon and the increase in interferon is the marker for TB. The IGRA is of more utility for diagnosing latent, rather than active, TB.
These tests are preferred to skin tests for people who have received BCG vaccine, but false-positive and false-negative results are both possible. The other advantage of an IGRA over a skin test is that it requires only a single visit.
Bacillus Calmette–Guérin (BCG) vaccine
A vaccine for TB has been available for almost a century. It is widely used around the world where it is often given to infants at birth. It doesn’t prevent TB but only reduces the risk. Its efficacy may be as low as 19%. It seems to have its greatest effect in preventing miliary tuberculosis or tuberculosis meningitis. It has never been used in the US where the prevalence of TB is low and where the preferred approach has been to detect and treat latent infections. People who were vaccinated with BCG vaccine can have positive skin tests afterwards, but that doesn’t mean they have active TB. However, many never develop a positive PPD or revert to negative after the BCG.
Neither the skin tests nor the IGRAs are sufficient to diagnose a person with active TB. A positive test might mean they could have active TB, but it might just indicate they have latent TB. People with latent TB are not contagious. About one in ten will later develop active TB. The risk of progression to active disease can be reduced by treating them with various short courses of anti-tuberculosis drugs. The risk is not totally eliminated. It is increased if their immune system becomes weakened or compromised in some way, for instance by HIV infection or by chemotherapy. According to the CDC:
A positive TB skin test or TB blood test only tells that a person has been infected with TB bacteria. It does not tell whether the person has latent TB infection or has progressed to TB disease. Other tests, such as a chest x-ray and a sample of sputum, are needed to see whether the person has TB disease.
While PCR to diagnose TB has been problematic, cell free DNA assays show great promise in diagnosing a host of infectious diseases, including TB, with a simple blood draw.
Conclusion: Don’t try to diagnose active tuberculosis with IGRAs
The advice of the WHO should be followed for TB serology. The currently available IGRAs are not sufficient by themselves for a diagnosis of active TB. IGRAs are the best test for latent TB and are part of the diagnostic armamentarium for trying to determine if the patient has active TB. Definitive diagnosis requires follow-up with other tests such as chest x-rays, sputum cultures and perhaps cell free DNA assays. At best, an IGRA might be used to help identify those who need more definitive testing. At worst, it is a waste of money and can misinform through false results.
This article was originally published in the Science-Based Medicine Blog.
