Some doctors are offering laser therapy for “vaginal rejuvenation”. It is no more effective than placebo, can cause harm, and is very expensive.
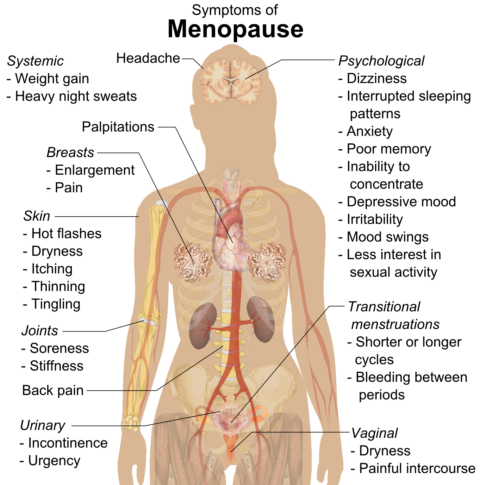
After menopause, the absence of estrogen may cause a number of symptoms. About half of women develop vulvovaginal atrophy (VVA). The lack of estrogen causes thinning and fragility of the vulvar and vaginal skin. Women with VVA have vaginal dryness, poor lubrication, painful intercourse, and urinary symptoms including incontinence and bladder infections. Hormone replacement therapy is an effective treatment. Estrogen can be provided topically in doses too small to cause systemic effects; but many women are reluctant to use hormones, and some have been advised by their doctors to avoid estrogens. Some gynecologists are offering laser therapy as an alternative.
An article published on Harvard Women’s Health Watch on October 1, 2021 said that laser therapy can counter the vaginal symptoms of menopause. They reported a small trial published in the journal Menopause in July 2021. It studied 25 women divided into two groups: one got topical estrogen, the other got laser therapy. The study found that “although vaginal estrogen performed better on certain measures, laser therapy is an effective treatment for vaginal atrophy as well”.
Less than 2 weeks later, a larger study showed that laser therapy was not significantly better than sham treatment. It was a randomized double-blind sham-controlled clinical trial of 85 patients in Australia (UNSW Sydney) and was published in The Journal of the American Medical Association (JAMA). The lowest possible laser setting (too low to have an effect) was used as the sham control, and both the laser group and the control group got the same local anesthesia. Participants in both groups got 3 treatments a month apart and were followed for 12 months. Biopsies were done and histology confirmed that there were no statistically significant differences between the two groups. In fact, “A shift from postmenopausal to premenopausal histology was found in two of 22 (9%) of participants in the treatment group and three of 24 (12.5%) in the sham group.”
The authors concluded:
The annual cost of laser treatment to the individual for management of vaginal menopausal symptoms was reported to be $2733, and because there is no demonstrable difference versus sham treatment, it cannot be considered to be cost-effective.
As reported by Heather Saxena in AusDoc magazine:
The findings have prompted two US obstetrician-gynaecologists from the University of Utah’s school of medicine to call for vaginal rejuvenation therapy to be restricted to research settings until high-quality evidence supported both effectiveness and safety. They wrote in an editorial that the widespread use of the therapy based on “highly optimistic short-term uncontrolled trials” followed by mounting reports of adverse events evoked a sense of deja vu as it was akin to the rush to market of vaginal mesh products before completion of rigorous trials. Although marketing prior to the availability of evidence demonstrating efficacy and safety may be associated with short-term profits for companies and clinicians, this approach closes any window of opportunity to actually learn what individuals, if any, benefit from the treatment, as well as those at increased risk for harms,’ they wrote.
Vaginal laser treatments are not alternative medicine but are used by mainstream MDs
Many MDs offer vaginal laser treatments. Here’s just one example. There are many others who offer vaginal rejuvenation with devices like Juliet, Renovalase, and Monalisa touch. Sciencebasedmedicine.org is an equal opportunity website: we don’t just criticize alternative medicine, we criticize conventional medicine when it is not based on good scientific evidence. Sometimes mainstream doctors get it wrong, and this is a prime example.
How is it supposed to work?
It is said to work by heating the tissue, improving blood flow, and stimulating regeneration. The cells are injured, and as they heal, they supposedly return to their healthy premenopausal state.
A clinic that offers vaginal rejuvenation explains:
As we age, the vaginal cells lose both collagen elastin. This unhealthy state cause a womens [sic] vaginal cells to become dry and inflexible. Eventually sex becomes very painful and for a vast number of women frankly impossible. The MonaLisa laser causes an injury to the cells lining the vagina. In an effort to heal this injury, the body sends in growth factors and stem cells which increase both collagen and elastin production in the cells. After three painless mona lisa treatments the vaginal cells are back to a normal healthy state and sex is once again painless and pleasurable.
There are insufficient placebo-controlled trials of energy-based therapies, including laser, to draw conclusions on efficacy and safety or to make treatment recommendations.
Does it work?
A 2020 systematic review concluded:
There are 3 randomized trials comparing energy-based systems with hormonal treatment, with no clinical difference in these 2 approaches. Although prospective data continue to show promising outcomes, without strong evidence from well-powered, double-blind placebo-controlled trials to determine the efficacy of treatment compared with placebo, the use of energy-based treatments should continue to be undertaken in research studies only, with high-quality studies essentially free from bias.
Is vaginal laser therapy safe?
The safety of this treatment is questionable. There have been reports of scarring, burning, and pain.
On July 30, 2018, the U.S. Food and Drug Administration (FDA) issued a warning about energy-based devices used to treat vaginal conditions and symptoms related to menopause, urinary incontinence, or sexual function. Currently, no vaginal laser device or procedure is cleared or approved by the FDA for any of these vaginal issues.
Conclusion: IMHO, not the best choice
Laser therapy for postmenopausal vaginal atrophy is no better than placebo, is much more expensive than topical estrogen, and may have serious side effects. Topical estrogen is proven to work, and in my opinion it is a much better choice.
This article was originally published in the Science-Based Medicine Blog.
Note: Thanks to Loretta Marron of Friends of Science in Medicine for suggesting I write about this and for providing helpful links.
